- Home
- About
- Treatments & Expertise
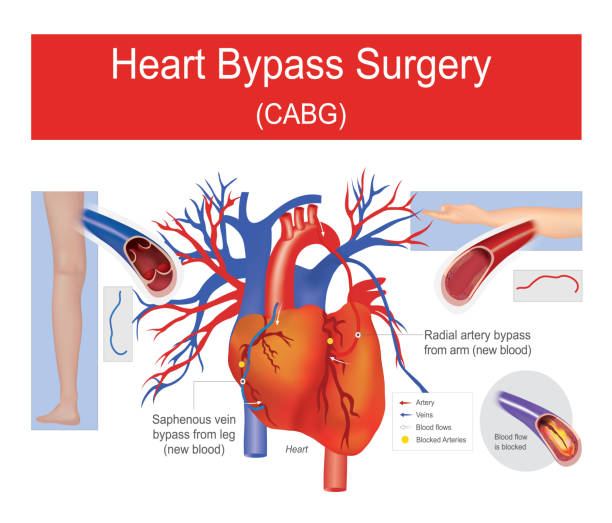
- Heart Bypass Surgery
- Mitral Valve Repair & Replacement Surgery
- Aortic Valve Repair & Replacement Surgery
- Tricuspid Valve Repair & Replacement Surgery
- Infective Endocarditis Surgery
- Redo Operations – 2nd & 3rd time Cardiac Surgeries
- Pericardiectomy
- TAVR – Transcatheter Aortic Valve Replacement
- Aortic Aneurysm Surgery
- Extracorporeal Membrane Oxygenation (ECMO) Therapy
- LVAD – Left Ventricular Assist Device
- Heart Transplant
- Lung transplant
- FAQs
- Gallery
- Testimonials
- Resources
- Publications
- Videos
- Contact
- Book an appointment